Chronic Pain and Depression: Understanding the Deep Connection
By: Saika J
Chronic pain, defined as pain persisting for more than three months, affects a significant portion of the global population. Recent studies have highlighted a strong association between chronic pain and an increased risk of depression. This article delves into the intricate relationship between these two conditions, exploring the underlying mechanisms, implications for treatment, and strategies for holistic management.
Prevalence of Chronic Pain and Depression
Approximately 30% of individuals worldwide experience chronic pain conditions such as low back pain, migraines, and fibromyalgia. Research indicates that individuals with chronic pain are up to four times more likely to develop depression compared to those without chronic pain. This co-occurrence significantly impacts daily functioning, quality of life, and overall well-being.
The Biological Link: Inflammation and Neural Disruption
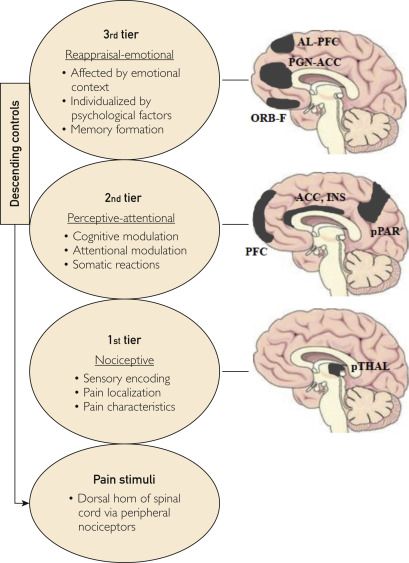
Emerging evidence suggests that systemic inflammation plays a pivotal role in the connection between chronic pain and depression. Elevated levels of inflammatory markers, such as C-reactive protein (CRP), have been observed in individuals suffering from both conditions. Chronic pain can lead to persistent activation of the immune system, resulting in neuroinflammation that affects mood regulation and cognitive functions.
Psychological and Social Factors
Beyond biological mechanisms, psychological and social factors contribute to the interplay between chronic pain and depression. The persistent discomfort and limitations imposed by chronic pain can lead to feelings of helplessness, social isolation, and reduced participation in enjoyable activities, all of which are risk factors for depression. Additionally, the stigma associated with chronic pain and mental health issues can exacerbate emotional distress.
Implications for Treatment
Understanding the bidirectional relationship between chronic pain and depression underscores the need for integrated treatment approaches. Healthcare providers are encouraged to adopt multidisciplinary strategies that address both physical and psychological aspects of these conditions. This may include:
-
Pharmacological Interventions: Utilizing medications that target both pain and depressive symptoms, such as certain antidepressants with analgesic properties.
-
Psychotherapy: Cognitive-behavioral therapy (CBT) has shown efficacy in managing chronic pain and associated depression by altering maladaptive thought patterns and promoting coping strategies.
-
Physical Therapy: Engaging in tailored exercise programs can improve physical function and mood.
-
Mind-Body Techniques: Practices like mindfulness meditation, yoga, and relaxation techniques can alleviate pain perception and enhance emotional well-being.
Preventive Measures and Lifestyle Modifications
Preventing the onset or exacerbation of depression in individuals with chronic pain involves proactive measures:
-
Regular Physical Activity: Engaging in low-impact exercises can reduce pain severity and improve mood.
-
Healthy Diet: Consuming an anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids may mitigate inflammation.
-
Sleep Hygiene: Ensuring adequate and quality sleep supports overall health and pain management.
-
Social Support: Maintaining strong social connections can buffer against the emotional toll of chronic pain.
Bottom-Line
The intricate relationship between chronic pain and depression necessitates a comprehensive understanding and approach to treatment. By recognizing the multifaceted nature of these conditions, individuals and healthcare providers can work collaboratively to implement effective strategies that address both physical discomfort and emotional distress, ultimately enhancing quality of life.