Diabetes and Your Skin: Unveiling the Hidden Clues
Beyond the Skin: A Holistic Approach to Diabetes Management
By: Saika J
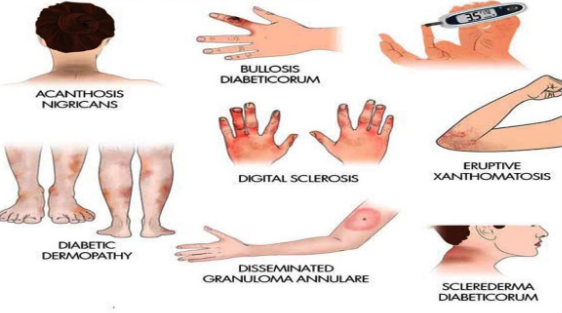
Diabetes, a chronic condition marked by high blood sugar levels, wreaks havoc on your body in numerous ways. While many associate diabetes with symptoms like excessive thirst, frequent urination, and fatigue, the impact can extend far beyond. Surprisingly, your skin can become a silent messenger, revealing hidden clues about your blood sugar control.
This article delves into five key warning signs of diabetes that manifest on your skin. By understanding these signs and seeking prompt medical attention, you can take proactive steps to manage your diabetes and prevent complications.
Unveiling the Connection: How High Blood Sugar Affects Your Skin
When your body struggles to effectively utilize sugar (glucose) for energy, it creates a domino effect. Excess sugar in the bloodstream damages blood vessels and nerves throughout your body, including those supplying your skin. This compromised circulation and nerve function can lead to a variety of skin problems.
Furthermore, high blood sugar creates a breeding ground for infections. The weakened immune system associated with diabetes struggles to fight off bacteria and fungi, making skin infections more frequent and persistent.
The 5 Skin Warning Signs of Diabetes:
1. Yellowish, Waxy Patches (Necrobiosis Lipoidica Diabeticorum):
Imagine reddish-brown, raised patches appearing on your shins, especially around the ankles. These patches may progress, becoming yellowish, waxy, and well-defined. This is Necrobiosis Lipoidica Diabeticorum (NLD), a relatively uncommon skin condition linked to diabetes. The exact cause remains unknown, but it’s believed to be associated with inflammation in blood vessels.
NLD can cause itching and discomfort, but the bigger concern lies in the underlying cause – poorly controlled diabetes. While NLD itself is not life-threatening, it signifies the need for immediate medical intervention to regulate blood sugar levels and prevent further complications.
2. Dark, Velvety Skin Patches (Acanthosis Nigricans):
Have you noticed dark, velvety patches of skin on your neck, armpits, or groin? These patches, often accompanied by a thickening of the skin, could be a sign of Acanthosis Nigricans (AN). This condition arises when the body produces an excess of insulin, a hormone responsible for driving sugar into cells.
While AN itself is not harmful, it often signals prediabetes or type 2 diabetes. It’s particularly prevalent in individuals with darker skin tones and those carrying excess weight. If you notice AN, schedule an appointment with your doctor to assess your blood sugar levels and receive appropriate treatment.
3. Recurrent Blisters (Diabetic Bullae):
Diabetic bullae are a rare but concerning skin manifestation of diabetes. These large, fluid-filled blisters typically appear on the hands, feet, fingers, or toes. Unlike regular blisters, they often develop suddenly and without any prior injury. Diabetic bullae are painless, but they can rupture easily, leading to secondary infections.
The exact cause of diabetic bullae remains unclear, but it’s believed to be linked to a combination of factors, including poor circulation, nerve damage, and immune system dysfunction. If you experience diabetic bullae, consult your doctor immediately. Early diagnosis and treatment are crucial to prevent complications and promote healing.
4. Slow-Healing Cuts and Sores:
One of the most common skin problems associated with diabetes is delayed wound healing. High blood sugar levels hinder the body’s ability to fight off infection and promote tissue repair. Even minor cuts, scrapes, or insect bites can take weeks or even months to heal completely, increasing the risk of developing serious infections.
If you notice any cuts, scrapes, or sores that seem to be taking an unusually long time to heal, see your doctor right away. Proper wound care, meticulous blood sugar management, and addressing underlying circulatory issues are essential for preventing further complications.
5. Ring-Shaped Rashes (Granuloma Annulare):
Granuloma annulare is a non-contagious skin condition characterized by raised, red or brown bumps arranged in a ring pattern. While it can affect anyone, it’s more common in young adults and can appear on the hands, feet, legs, or trunk.
Although the exact cause of granuloma annulare remains unknown, research suggests a potential link between this condition and diabetes, particularly type 2 diabetes. In some cases, minor skin injuries or certain medications used to manage diabetes might trigger granuloma annulare.
While granuloma annulare itself is not harmful, it can cause emotional distress due to its appearance. Consulting a dermatologist can help determine the best course of treatment, which may involve topical steroid creams or other medications.
These five skin warning signs serve as valuable clues for identifying potential diabetes or poorly managed existing diabetes. However, early detection and diagnosis are key to preventing complications. Here’s what you can do:
-
Schedule a doctor’s appointment: If you notice any of the skin signs mentioned above, don’t hesitate to schedule an appointment with your doctor. They will perform a comprehensive evaluation, including a physical examination, blood tests to measure your blood sugar levels, and potentially other tests to confirm or rule out diabetes.
-
Embrace proactive blood sugar management: Once diagnosed with diabetes, working closely with your doctor to create a personalized diabetes management plan is crucial. This plan may involve a combination of strategies, such as:
- Dietary modifications: Adopting a healthy eating pattern that prioritizes whole foods, fruits, vegetables, and lean proteins while limiting processed foods, added sugars, and unhealthy fats can significantly improve blood sugar control.
- Physical activity: Engaging in regular physical activity helps your body utilize sugar more efficiently. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Medications: Depending on the type and severity of your diabetes, your doctor may prescribe medications like oral medications or insulin to help regulate your blood sugar levels.
-
Practice meticulous foot care: Diabetes can increase your risk of foot problems, including neuropathy (nerve damage) and poor circulation. These complications can lead to undetected cuts, ulcers, and even infections that may require amputation in severe cases. Here are some essential foot care tips:
- Inspect your feet daily for any cuts, scrapes, blisters, or signs of infection.
- Wash your feet daily with warm, soapy water and dry them thoroughly, especially between the toes.
- Moisturize your feet regularly to prevent cracks and dryness.
- Wear comfortable, well-fitting shoes with good arch support and adequate cushioning.
- Schedule regular foot examinations with your doctor.
-
Prioritize stress management: Chronic stress can elevate blood sugar levels and make it more difficult to manage diabetes. Explore healthy stress-management techniques like yoga, meditation, deep breathing exercises, or spending time in nature.
-
Seek support: Living with diabetes can be challenging. Don’t hesitate to seek support from a registered dietitian, diabetes educator, or a support group. Connecting with others who understand your journey can provide invaluable encouragement and guidance.
Living a fulfilling life with diabetes is possible. By recognizing the skin signs, taking proactive steps toward managing your blood sugar, and embracing a healthy lifestyle, you can significantly reduce your risk of complications and live a long, healthy life.
Remember:
-
This article provides general information and should not be considered a substitute for professional medical advice. Always consult with your doctor for diagnosis and treatment recommendations tailored to your specific needs.
-
Early detection and management are crucial for preventing diabetes complications.
-
A holistic approach that combines healthy lifestyle choices with proper medical care empowers you to thrive with diabetes.
While significant progress has been made in understanding diabetes and its impact on the body, the link between diabetes and certain skin conditions remains an evolving area of research. Here’s a glimpse into ongoing efforts to unveil the mysteries behind these skin warning signs:
-
Investigating the Underlying Causes: Researchers are actively exploring the precise mechanisms by which high blood sugar levels and diabetes contribute to specific skin conditions. This deeper understanding will pave the way for the development of targeted treatment strategies. For instance, research on Necrobiosis Lipoidica Diabeticorum focuses on the role of inflammation in blood vessels, while studies on Acanthosis Nigricans delve into the connection between insulin resistance and skin cell changes.
-
Exploring the Role of Genetics: Genetics likely plays a role in how individuals with diabetes experience skin manifestations. Identifying specific genetic markers associated with these conditions could offer valuable insights for personalized treatment approaches.
-
Developing Early Detection Tools: The ultimate goal is to leverage the knowledge of diabetes-related skin signs for early detection and intervention. Researchers are exploring the possibility of using non-invasive imaging techniques or specific biomarkers in the skin to identify individuals at risk of developing diabetes or experiencing complications.
The Future Holds Promise:
The ongoing research efforts hold immense promise for improving the lives of those living with diabetes. Here’s what we can potentially look forward to:
-
More Targeted Treatments: A deeper understanding of the underlying causes of diabetes-related skin conditions could lead to the development of more targeted and effective treatments. For example, this might involve medications that specifically address inflammation in blood vessels or therapies that regulate insulin signaling in skin cells.
-
Improved Prognosis and Prevention: The ability to identify individuals at risk of developing diabetes through early detection of skin signs could lead to earlier intervention and potentially prevent the progression of the disease itself.
-
Enhanced Quality of Life: By effectively managing both the internal and external aspects of diabetes, individuals can experience a significant improvement in their overall quality of life. Addressing skin concerns associated with diabetes not only promotes physical well-being but also reduces the emotional distress caused by these conditions.
Bottom-line: While diabetes can cast a long shadow on your health, it doesn’t have to define your life. By being aware of the skin warning signs, taking a proactive approach to diabetes management, and staying informed about the latest research advancements, you can empower yourself to navigate this journey with knowledge, confidence, and hope. Remember, you are not alone. With the right support system and a commitment to healthy living, you can thrive despite having diabetes.
Disclaimer: Tips and suggestions mentioned in the article are for general information purposes only and should not be construed as professional medical advice. Always consult your doctor or a dietician before starting any fitness programme or making any changes to your diet.

